Trigger Finger
What is trigger finger?
Trigger finger is a condition that affects the tendons responsible for flexing the fingers and thumb, which causes them to lock or catch when the digit is bent or straightened. This condition is also known as stenosing tenosynovitis and can affect any of the digits, but is most common in:
The ring finger
The thumb (often known as trigger thumb)
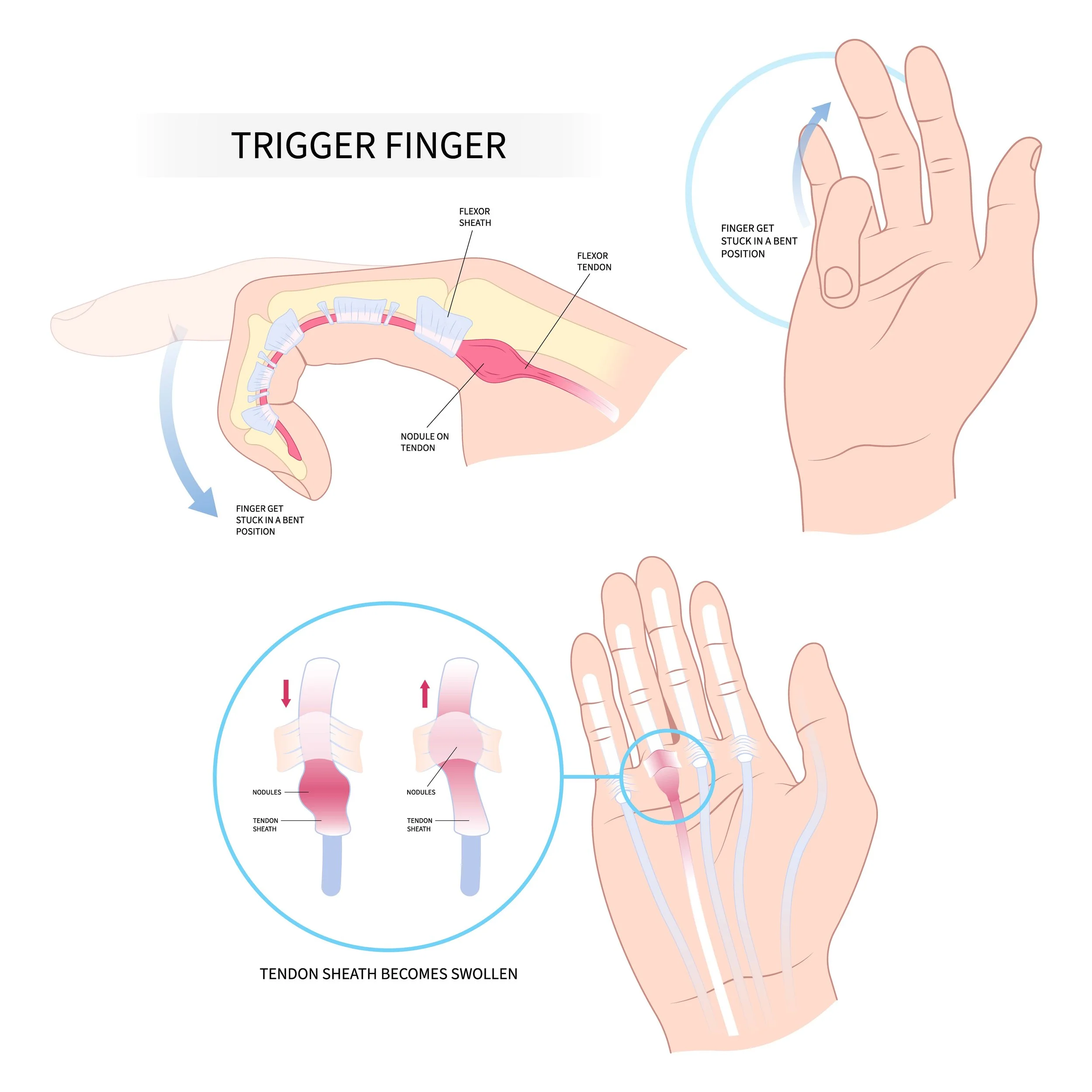
Trigger finger occurs when the tendon sheath that surrounds the tendon gets inflamed, making it harder for the tendon to glide through the tendon pulleys which form a ‘tunnel’ as the digit bends. Over time, the tendon may also become inflamed and develop a small nodule on the surface, further aggravating the condition. When the digit bends or straightens, the nodule must pass through the sheath ‘tunnel’, which causes a sensation of catching or popping.
In severe cases of trigger finger, the digit locks and becomes stuck in a bent position and the patient must use their other hand to manually straighten the finger or thumb.
Several factors are known to increase a person’s risk of developing trigger finger, including:
Medical conditions, such as diabetes or rheumatoid arthritis.
Forceful hand activities.
Age. Trigger finger is more common in older individuals and is rare in children.
Symptoms of a trigger finger
Most trigger fingers come on gradually without a clear injury, although they may follow a period of extensive hand use. Symptoms tend to be worse after period of inactivity and may include:
A tender lump at the base of the affected digit on the palm side of the hand
A catching, popping or locking sensation with finger or thumb movement
Pain with movement of the digit
How Ben can help?
Diagnosing trigger finger
Ben will typically be able to diagnose trigger finger by talking to you about your symptom and examining your hand. Ben assess whether there is tenderness of the sheath ‘tunnel’ by applying gentle pressure to the palm of your hand. He will also look for thickening or swelling of the sheath at the base of your affected finger or thumb, and he will feel and/or listen for a clicking or catching sensation on movement of your affected digit.
Treating a ganglion
Non-surgical treatment
Immobilisation
Activity can make trigger finger worse and therefore Ben may recommend a splint to minimise movement and keep the finger or thumb in a straight position. Following this, gentle stretching exercises may be recommended to decrease stiffness and improve the range of motion in the affected digit.
Steroid injections
Powerful anti-inflammatory agents, such as cortisone (corticosteroid) can be injected into the sheath of the affected digit, to improve the condition. Sometimes a second injection is recommended if the first one didn’t help, however after this, surgery will usually be recommended.
Surgical treatment
Ben will usually recommend surgery if non-surgical treatments have been unsuccessful or if you have complete loss of function in your digit. The surgery is called a trigger finger release and involves releasing the tendon sheath so the tendon can glide freely. Surgery is usually performed through a small incision in the palm of the hand and the sheath is divided to alleviate the clicking/catching sensation. While this sheath will be damaged by the surgery, there is usually no impact to your overall hand functionality because the other sheaths compensate.
Patients can usually go home on the same day as their surgery. You can expect to feel some tenderness, discomfort and swelling after surgery, but usual activities can typically resume within 4 to 6 weeks, however stiffness may remain for up to 6 months.
The vast majority of patients experience significant improvement after a trigger finger release, however full range of motion may not fully be restored if there was complete dysfunction of the finger or thumb prior to intervention.
-
Ben operates at multiple hospitals across Melbourne’s bayside and peninsula region, including:
Linacre Private Hospital, Hampton
Peninsula Private Hospital, Langwarrin
The Bays Private Hospital, Mornington
He can discuss your preferences in person during your consultation.
-
Ben will see you for a post-operative appointment usually 2 weeks after your surgery. During this appointment he will asses your wound and check that healing and mobility is progressing as expected. There will be no cost for this appointment.
As well as this, Ben will usually refer you to a hand therapist, who focuses on rehabilitation after an injury, and will work with you to improve function of the affected area.
-
You can usually start driving again 4-6 weeks after the operation. However, every surgery is different, so Ben will provide individualised advice as part of the initial consultation.