Carpal tunnel syndrome
What is carpal tunnel syndrome?
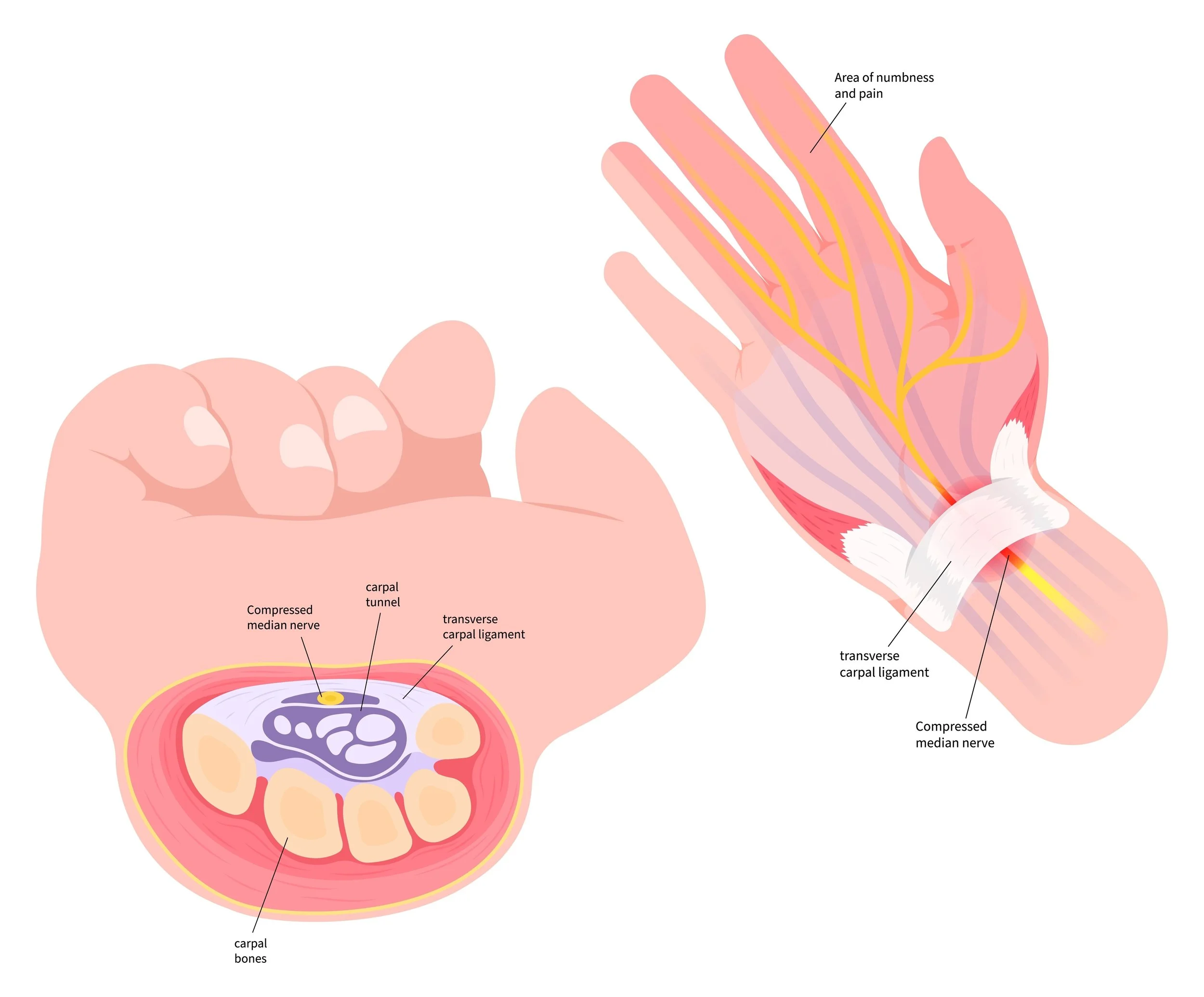
Carpal tunnel syndrome is a common condition that occurs when one of the main nerves of the hand is compressed as it travels through the wrist. It causes numbness, tingling and/or pain in the hand and forearm and can lead to permanent dysfunction of the hand if not diagnosed and treated quickly.
The carpal tunnel refers to the narrow passageway in the wrist that houses all the tendons and nerves that control the hand. Carpal tunnel syndrome occurs when this passageway is reduced in size, or when the tissues surrounding the tendons swells, putting pressures on the main nerve that supplies the hand - the median nerve.
There are many causes of carpal tunnel syndrome and often it’s a combination of factors that lead to the median nerve being compressed, however it has been found to be more common in women and the elderly. Risk factors include:
Genetics - the carpal tunnel is naturally smaller in some people, which means there is less space for the median nerve in some individuals. This usually runs in families
Repetitive hand use - repeating the same hand or wrist activities for a long period of time may cause the tendons in the wrist to swell, which in turn puts pressure on the median nerve.
Hand and wrist position - if the hand and wrist is flexed or extended for prolonged periods of time it can increase the pressure on the median nerve.
Pregnancy - Swelling is more common during pregnancy due to hormonal changes, and this can cause compression of the median nerve.
Health conditions - carpal tunnel syndrome is more common if you suffer from diabetes, rheumatoid arthritis and/or thyroid gland imbalance.
How do I know if I have carpal tunnel syndrome?
In most cases, the symptoms of carpal tunnel syndrome develop slowly without a specific injury, however as the condition worsens one or more of the following symptoms may persist for long periods of time. These symptoms are often first noticed at night:
Numbness, tingling, burning and pain - most notably in the thumb, index, middle and ring fingers. This feeling may also travel up the forearm towards the shoulder.
Shock-like sensations felt through the thumb, index, middle and ring fingers.
Weakness in the hand - you may find fine motor movements (eg. buttoning up a shirt) hard, or you may find you are dropping things more regularly.
How Ben can help?
Diagnosing carpal tunnel syndrome
Ben will first chat to you about your general health, medical history and what symptoms you are experiencing. He will then use two methods to diagnose carpal tunnel syndrome:
Physical Examination: Ben will examine your hand and wrist and perform several tests to ascertain whether there is tingling, numbness and/or weakness. These tests include tapping along your median nerve on the palm side of your hand/wrist; bending and holding your wrist in a flexed position; testing sensitivity in your fingertips while your eyes are closed; and checking for weakness and/or atrophy of muscles around your thumb.
Further Investigation: While physical examinations are often enough to diagnose carpal tunnel syndrome, Ben may order further tests in certain circumstances. Nerve conduction studies (NCS) and Electromyogram (EMG) measure how well your nerves are working and help to diagnose how severe the median nerve is compressed and if there are other structures affected. Ultrasounds may be ordered to evaluate the median nerve for signs of compression. An X-ray provides images of bones and may be ordered to rule out other causes of your symptoms. Finally a magnetic resonance imaging (MRI) scan may be ordered if Ben needs a better image of the body’s soft tissues than what an X-ray can give. It can help identify abnormal tissues that may be impacting the median nerve, or help Ben determine if there are issues with the nerve itself (i.e. a tumour or nerve scarring).
Treating carpal tunnel syndrome
Non-surgical treatment
Non-surgical treatment is generally offered when the symptoms of carpal tunnel syndrome are mild or if the diagnosis is inconclusive.
Ben may recommend bracing or splinting the wrist overnight to limit bending while you sleep. This reduces pressure on the nerve in the carpal tunnel and can therefore reduce the symptoms.
If your symptoms are brought on by particular activities you do recreationally or at work, Ben may recommend modifying how you perform the task/s to limit the amount of time your wrist is flexed or extended.
In some cases, Ben may suggest medication to help treat carpal tunnel syndrome. Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can help to relieve inflammation. Steroid injections (cortisone) can also be injected into the carpal tunnel to relieve symptoms. Both medications, however, typically only provide temporary relief.
In conjunction with these non-surgical treatment options, Ben will usually refer you to a hand therapist who will develop an exercise plan with you to help the median nerve move more freely through the carpal tunnel, thus reducing symptoms.
Surgical treatment
Ben will usually recommend surgery if the non-surgical treatment options fail to provide relief. The goal of surgery is to relieve pressure on your median nerve by cutting the ligament that forms the roof of the tunnel (transverse carpal tunnel ligament), which increases the size of the carpal tunnel. This surgical process is known as a ‘carpal tunnel release’.
Ben performs the operation both endoscopically (key hole) and open via a small incision on the palm of your hand so he can access and divide the transverse carpal tunnel ligament. Usually this procedure is done on an outpatient basis, where you will be given general anaesthesia, but will be able to go home the same day.
You will be asked to elevate your hand above your heart and move your fingers immediately after surgery. This helps to reduce swelling and prevent stiffness.
In most cases you will need to wear a splint for two weeks after surgery. Hand therapy is usually also recommended to maximise your recovery and ensure optimal strength is regained.
Patients usually notice improvement in their symptoms within the first 1-2 weeks, particularly overnight, however, it can take up to one year for for patients to make a complete recovery.
-
Ben operates at multiple hospitals across Melbourne’s bayside and peninsula region, including:
Linacre Private Hospital, Hampton
Peninsula Private Hospital, Langwarrin
The Bays Private Hospital, Mornington
He can discuss your preferences in person during your consultation.
-
Ben will see you for a post-operative appointment usually 2 weeks after your surgery. During this appointment he will asses your wound and check that healing and mobility is progressing as expected. There will be no cost for this appointment.
As well as this, Ben will usually refer you to a hand therapist, who focuses on rehabilitation after an injury, and will work with you to improve function of the affected area.
-
You can usually start driving again 4-6 weeks after the operation. However, every surgery is different, so Ben will provide individualised advice as part of the initial consultation.