Hand Arthritis
What is hand arthritis?
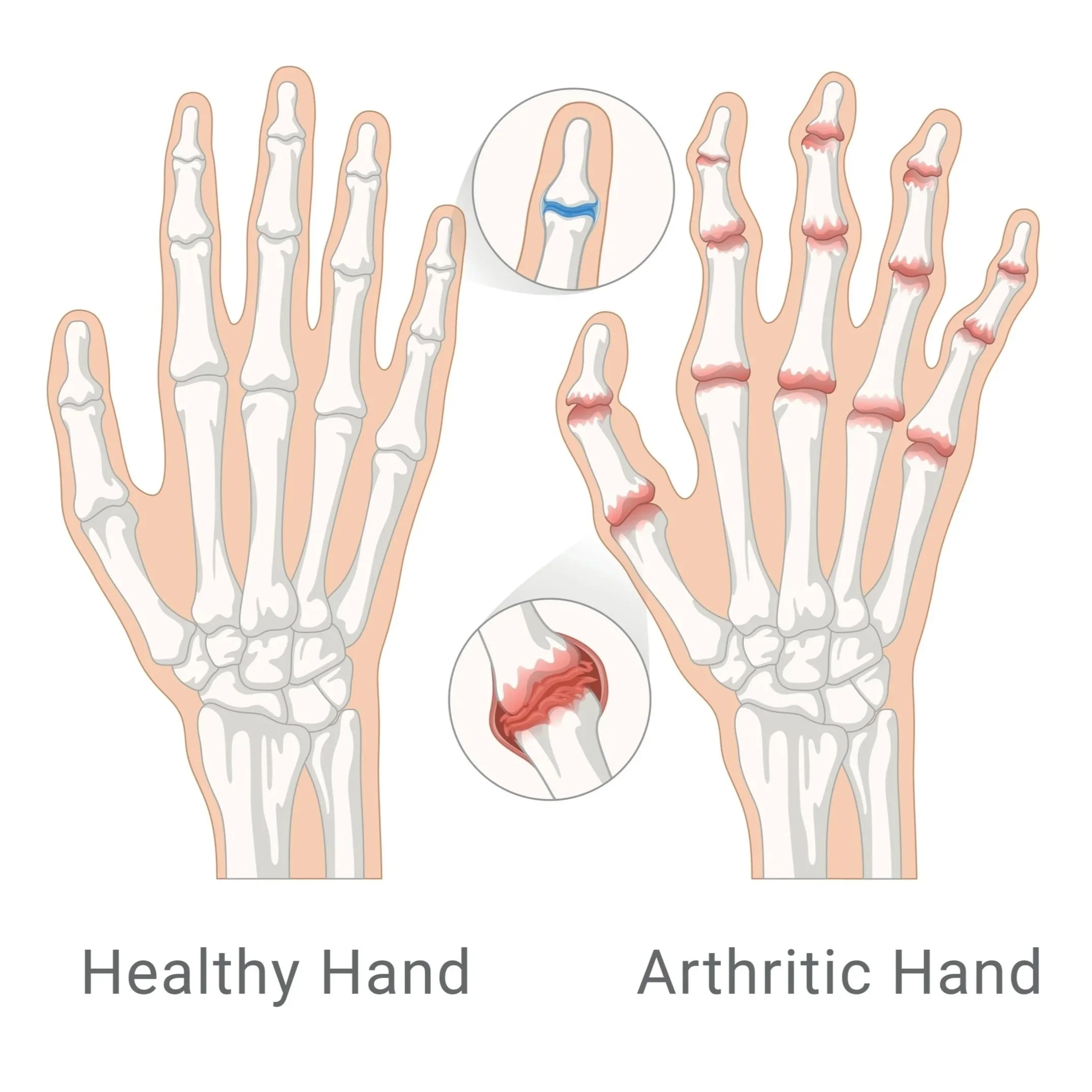
Arthritis is defined as the inflammation of one or more of your joints. It occurs when the cartilage between your joints breaks down, resulting in there no longer being a smooth gliding surface for the bones to move. Arthritis of the hands is a common condition that can be functionally quite limiting because of the pain it causes.
The two most common forms of arthritis are osteoarthritis and rheumatoid arthritis.
Osteoarthritis is the degenerative ‘wear and tear’ form of the disease that generally affects older people and typically appears in a predictable pattern in certain joints, most notably in the hands.
Rheumatoid arthritis, by contrast, is a chronic autoimmune disease that causes swelling of the joint lining, which in turn, damages the cartilage over time. It can affect people in a wider age range and can be diagnosed through a blood test..
Symptoms of a hand arthritis
Arthritis can affect any joint in the hand and causes the following symptoms:
Pain: In the early stages of hand arthritis, you may notice a dull or burning sensation in the affected joint, which can often intensify after periods of increased joint use. As the cartilage wears away, you will notice the pain occur more frequently, and it is worse in the morning and/or with changes in weather.
Swelling: The affected joints often swell after prolonged of heavy use.
Stiffness: There is often reduced range of motion in the affected joints that is more noticeable when you first wake up in the morning.
Warmth: The joint may feel warm to touch due to the body’s inflammatory response working in overdrive. This is more common with rheumatoid arthritis.
Nodes or bony lumps: The joints may appear larger than normal due to a combination of bone changes and/or loss of cartilage. The joints may also have developed small mucosal cysts that cause ridging in the nail plate of the affected finger.
How Ben can help?
Diagnosing hand arthritis
Ben will typically be able to diagnose hand arthritis and/or assess whether surgical intervention is required by examining the hand and by taking X-rays.
Treating hand arthritis
Non-surgical treatment
There are a myriad of non-surgical treatments for hand arthritis that will normally be recommended before surgical intervention. Usually these will be recommended by your GP and only once these treatments have been exhausted will a referral to Ben be necessary. These options include:
Medication
Splinting of the affected digits
Activity modification
Injections
Ice/heat
The non-surgical treatment option/s recommended to you will be based on:
How far the arthritis has progressed
How many joints are involved
Your age, activity level and other medical conditions
Whether your dominant or non-dominant hand is affected
Your personal goals, home support structure, and ability to understand the treatment and comply with a therapy program
Surgical treatment
Ben will usually recommend surgery if non-surgical treatments have failed to provide pain relief. Surgery will be different for every patient and will depend on which digits/joints are affected and how far the arthritis has progressed. If there is any way the joint can be preserved, this surgical option will be offered to you and the tailored surgical approach will be explained to you by Ben during your consult.
If however, preservation of the joint is not possible because the surfaces no longer work, there are two main surgical options:
Joint Fusion (arthrodesis) - this will offer pain relief because the damaged joint surfaces are gone, but there will no longer be joint motion. This will be less important for some joints, while for other joints, a fusion may significantly impact quality of life.
Joint Replacement - This surgical option will reduce pain while maintaining joint function and is usually recommended for joints where loss of motion will significantly impact quality of life. Ben will discuss with you, during your consultation, what material will be used for your individual replacement (usually ceramic or long-wearing metal) and the likely long-term outcomes for your specific situation. For sufferers of thumb arthritis, it is important to note that Ben is one of the only surgeons in the Bayside and Mornington Peninsula regions of Melbourne to offer thumb joint replacements.
-
Ben operates at multiple hospitals across Melbourne’s bayside and peninsula region, including:
Linacre Private Hospital, Hampton
Peninsula Private Hospital, Langwarrin
The Bays Private Hospital, Mornington
He can discuss your preferences in person during your consultation.
-
Ben will see you for a post-operative appointment usually 2 weeks after your surgery. During this appointment he will asses your wound and check that healing and mobility is progressing as expected. There will be no cost for this appointment.
As well as this, Ben will usually refer you to a hand therapist, who focuses on rehabilitation after an injury, and will work with you to improve function of the affected area.
-
You can usually start driving again 4-6 weeks after the operation. However, every surgery is different, so Ben will provide individualised advice as part of the initial consultation.