Scaphoid fractures
What is a scaphoid fracture of the wrist?
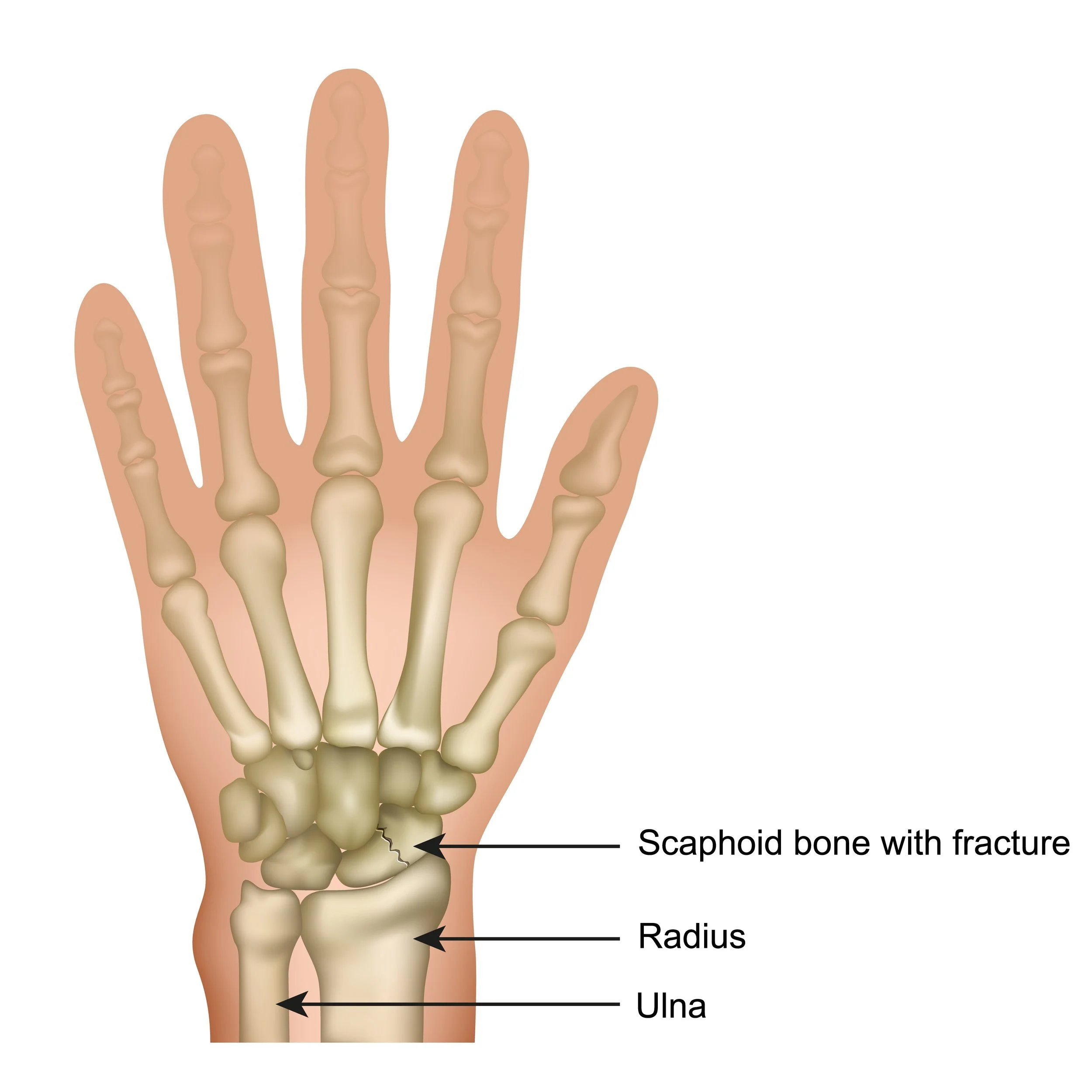
The scaphoid bone is one of the eight carpal bones in your wrist and is the one that is most commonly fractured, usually due to a fall on an outstretched hand. The location of the break in the bone can be categorised as follows, and this, along with whether the bone is displaced or not, determines how it will be fixed:
Distal pole fracture (closer to the thumb)
Waist fracture (middle of the bone)
Proximal pole fracture (closer to the forearm)
Displaced fractures are when the fragments of the bone have moved or slipped from their original position and usually require surgical intervention. In contrast, non-displaced fractures can often be treated with a cast or splint. However, given that parts of the scaphoid bone have poor blood supply, certain non-displaced fractures may still require surgery to minimise the chance of complications during the healing process.
How do I know if my scaphoid is fractured?
There is usually pain and swelling/bruising of the thumb, hand or wrist after a scaphoid fracture has occurred. There is also often tenderness when the base or side of the thumb (anatomically known as the snuffbox) is touched. Furthermore, moving your wrist or trying to grip, lift, push or pull objects may cause pain.
Usually there is no physical deformity with a scaphoid fracture, and it’s for this reason that you are encouraged to see a doctor if your wrist pain does not go away within a day of the injury taking place.
How Ben can help?
Diagnosing scaphoid wrist fractures
Ben will first chat to you about how your injury happened and what symptoms you are feeling. He will then use two methods to diagnose your fracture:
Physical Examination: Ben will examine your wrist and ascertain whether there is tenderness directly over the scaphoid in the anatomic snuffbox. He will also look for swelling, bruising and/or loss of motion in your wrist and/or thumb.
Imaging tests: Ben will most likely order X-rays to determine if the scaphoid is indeed fractured as well as if the bone fragment is displaced. In some cases, a scaphoid fracture does not immediately show up on a X-ray. If this is the case, Ben may recommend you wear a wrist splint for a period of time before returning for a follow-up X-ray. Magnetic resonance imaging (MRI) scans and/or computerised tomography (CT) scans may also be ordered by Ben if he wants to learn more about the bones and soft tissues in your wrist and to decide on the best treatment plan.
Treating scaphoid fractures
Non-surgical treatment
Non-surgical treatment is generally offered when the scaphoid bone is non-displaced, however the treatment will be different depending on where in the bone the fracture occurred:
Non-displaced scaphoid fractures near the thumb - given this part of the scaphoid bone (distal pole) has good blood supply, these types of fractures usually heal well with restricted activity and proper protection. As such, Ben will usually place your forearm in a cast or a splint that starts below your elbow and includes your thumb.
Non-displaced scaphoid fracture near the forearm - The blood supply is poor to both the the middle (waist) and end of the scaphoid bone closest to the forearm (proximal pole), often making healing more complicated. Typically healing is slower for this type of fracture so you can expect to be in a cast for longer than for a distal pole fracture. The cast starts below your elbow and finishes at the thumb. It needs to be worn for at least 8 weeks.
It is common for the fracture to be stiff after it heals, due to the lack of use. As such, Ben will usually refer you to a hand therapist to improve your range of motion.
Surgical treatment
Ben will recommend surgery if the scaphoid bone needs to be re-aligned and/or if the scaphoid is broken at the waist or proximal pole (i.e closer to the forearm). The goal of surgery is to stabilise the fracture and ensure it is given the best chance to heal.
He will typically use small screws, plates and/or wires to hold the fractured bones together. Sometimes these devices will stay on or in your bone for life, but in other cases, they will need to be removed after the fracture heals.
The size and location of the surgical incision will depend on the severity of the fracture, as well as where the scaphoid bone was broken. Typically, the more displaced the fragment, the bigger the incision will be. The incision may be made on either the palm side or the back of your wrist.
Scaphoid fractures of the wrist tend to heal slower than other bones in the body due to the low blood supply. As such, whether the treatment was surgical or non-surgical, you may be required to wear a cast or splint for up to 6 months. During this time, you will not be able to lift, carry, push, pull or throw with your injured wrist, and you must not partake in contact sports or in activities that risk you falling onto your hand.
Hand therapy is usually always recommended to maximise the chance of regaining full range of motion and strength, however some patients never return to their pre-injury state. Ben will discuss this with you during your consultation.
-
Ben operates at multiple hospitals across Melbourne’s bayside and peninsula region, including:
Linacre Private Hospital, Hampton
Peninsula Private Hospital, Langwarrin
The Bays Private Hospital, Mornington
He can discuss your preferences in person during your consultation.
-
Ben will see you for a post-operative appointment usually 2 weeks after your surgery. During this appointment he will asses your wound and check that healing and mobility is progressing as expected. There will be no cost for this appointment.
As well as this, Ben will usually refer you to a hand therapist, who focuses on rehabilitation after an injury, and will work with you to improve function of the affected area.
-
You can usually start driving again 4-6 weeks after the operation. However, every surgery is different, so Ben will provide individualised advice as part of the initial consultation.